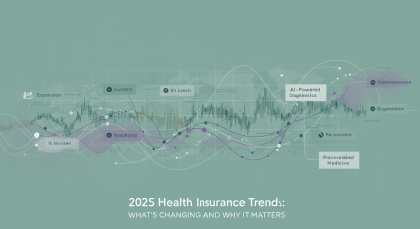
The health insurance landscape is undergoing unprecedented transformation in 2025, driven by technological advancement, regulatory changes, and evolving consumer expectations. As we navigate this pivotal year, understanding these emerging trends is crucial for consumers, employers, and healthcare providers alike. The convergence of artificial intelligence, climate-related health risks, and changing workforce dynamics is reshaping how health insurance operates and delivers value to millions of Americans.
The AI Revolution in Health Insurance
Transforming Claims Processing and Decision-Making
Artificial intelligence has emerged as the most significant disruptor in health insurance operations this year. Major insurers like Elevance, which covers about 110 million people, have rolled out generative AI models to 50,000 employees, while Centene Corp is using AI to manage contracts with medical groups and measure their performance. This widespread adoption represents a fundamental shift in how insurance companies process claims, assess risk, and make coverage decisions.
The integration of AI promises to streamline operations and reduce administrative costs, but it also raises important questions about transparency and fairness in healthcare decision-making. In 2025, insurers are tapping into AI to accelerate their claims and underwriting processes, with the end goal of helping customers start their policies faster and access their benefits quicker. However, the technology is not without controversy, as evidence suggests some applications may delay or limit necessary healthcare services.
Regulatory Response and Patient Protection
The rapid deployment of AI in health insurance has prompted significant regulatory action. California has taken the lead with groundbreaking legislation that ensures medical treatment decisions remain with licensed healthcare providers rather than being solely determined by AI algorithms. The new Physicians Make Decisions Act ensures that decisions about medical treatments are made by licensed health care providers, not solely determined by artificial intelligence algorithms used by health insurers.
This regulatory development signals a broader trend toward balancing technological innovation with patient protection. As AI becomes more prevalent in health insurance, consumers can expect more states to implement similar safeguards to ensure that automated systems enhance rather than replace human medical judgment.
Customer Experience as the New Battleground
Rising Expectations for Personalized Service
The emphasis on enhancing the customer experience in health care will be paramount in 2025, as companies like Apple, Netflix, and Amazon have conditioned consumers to expect personalized and seamless experiences. This shift represents a fundamental change in how health insurers approach their relationship with members, moving from a transaction-based model to one focused on ongoing engagement and support.
Health insurers are investing heavily in omnichannel customer experiences, mobile-first platforms, and personalized communication strategies. The expectation is that insurance interactions should be as intuitive and convenient as ordering products online or streaming entertainment content. This trend is driving insurers to redesign their digital platforms, improve mobile applications, and implement AI-powered chatbots for instant customer support.
Digital-First Service Delivery
The pandemic accelerated the adoption of digital health services, and 2025 sees this trend reaching maturity. Virtual care options, telehealth integration, and digital wellness programs are becoming standard offerings rather than optional add-ons. Insurers are partnering with technology companies to provide comprehensive digital health ecosystems that include everything from symptom checkers to prescription delivery services.
This digital transformation extends beyond member-facing services to include provider interactions. Electronic prior authorization systems, digital claims submission processes, and real-time benefit verification are becoming the norm, reducing administrative burden and improving care delivery efficiency.
Climate Change and Health Insurance Coverage
Expanding Coverage for Climate-Related Health Risks
Insurers may expand coverage to include health risks linked to natural disasters, with an emphasis on preventive care and post-disaster mental health services, and may develop new products aimed at addressing emerging health issues, such as vector-borne diseases. This represents a significant shift in how health insurers assess and manage risk in an era of increasing climate volatility.
The growing frequency and intensity of extreme weather events are creating new categories of health risks that traditional insurance models weren’t designed to address. Heat-related illnesses, respiratory problems from wildfire smoke, and mental health impacts from climate disasters are becoming more common and costly to treat.
Innovation in Risk Assessment
Climate change is forcing insurers to develop more sophisticated predictive models that account for environmental factors in health risk assessment. This includes analyzing geographic data, air quality indices, and weather patterns to better understand how environmental conditions affect population health and healthcare utilization patterns.
Insurance companies are also investing in prevention-focused programs that help communities prepare for climate-related health challenges. This includes everything from heat illness prevention education to mental health support for disaster-affected areas.
Medical Cost Trends and Premium Pressures
Rising Pharmaceutical Costs
Medical cost trends will continue to rise, with pharmaceutical costs, GLP-1s and other specialty drugs increasing in cost and utilization. The introduction of new weight-loss medications like GLP-1 receptor agonists represents a significant cost driver for health plans, as these medications can cost thousands of dollars per month and are increasingly prescribed for both diabetes and weight management.
Specialty drugs continue to represent a disproportionate share of pharmaceutical spending, with many new therapies carrying price tags of $100,000 or more per year. This trend is forcing insurers to develop more sophisticated drug management strategies, including value-based contracts with pharmaceutical companies and enhanced utilization management programs.
Impact on Premium Calculations
The rising cost of medical care is directly translating into higher premiums for consumers. Health Trends 2025 highlights costly cancer claims, mental health needs, and rising medical costs, requiring employers and insurers to adapt their response to innovative treatments and explore new plan management options. This creates a challenging environment where insurers must balance affordability with comprehensive coverage.
Insurers are responding by developing more sophisticated actuarial models that better predict costs and by implementing innovative cost-containment strategies. These include centers of excellence programs for high-cost procedures, bundled payment arrangements, and enhanced care management for chronic conditions.
Workforce Changes and Benefits Evolution
Post-Pandemic Employment Patterns
The transformation of work patterns following the COVID-19 pandemic continues to influence health insurance offerings in 2025. Remote work, hybrid arrangements, and the gig economy have created new challenges and opportunities for health benefits delivery. Employers are seeking more flexible benefit arrangements that can accommodate distributed workforces and varying employment patterns.
This shift is driving innovation in benefit design, with more emphasis on portable benefits, direct primary care arrangements, and digital health solutions that work regardless of geographic location. The traditional model of employer-sponsored insurance tied to specific work locations is evolving to meet the needs of a more mobile workforce.
Mental Health Integration
Mental health coverage has moved from a compliance requirement to a strategic priority for health plans. The ongoing mental health crisis, exacerbated by the pandemic and economic uncertainty, has led to significant increases in utilization and costs for mental health services. Insurers are responding by expanding provider networks, reducing barriers to care, and integrating mental health services with primary care.
The integration extends to workplace wellness programs, with employers and insurers collaborating on comprehensive mental health support that includes everything from stress management resources to crisis intervention services.
Technology Integration and Data Analytics
Advanced Analytics for Population Health
Health insurers are leveraging big data and advanced analytics to better understand population health trends and predict future healthcare needs. This includes analyzing social determinants of health, claims patterns, and environmental factors to develop more targeted interventions and prevention programs.
The use of predictive analytics is becoming more sophisticated, with insurers developing models that can identify high-risk members before they develop serious conditions. This enables early intervention strategies that can improve health outcomes while reducing long-term costs.
Interoperability and Data Sharing
The push for better data interoperability is gaining momentum in 2025, with new regulations and industry initiatives aimed at improving the flow of health information between providers, insurers, and patients. This improved data sharing enables better care coordination, reduces duplicate testing, and helps insurers make more informed coverage decisions.
The implementation of electronic health record integration and real-time data exchange is making it easier for insurers to process claims, verify medical necessity, and support care management activities.
Regulatory Landscape Changes
ACA Market Dynamics
The premium assistance tax credits that help reduce the cost of health coverage purchased through the Affordable Care Act’s public insurance exchanges were enhanced in 2021 and helped increase the number of enrollees to 21.4 million in 2024, but the enhancements are set to expire at the end of 2025. This potential policy change could significantly impact the individual insurance market and increase the number of uninsured Americans.
The uncertainty around subsidy continuation is creating planning challenges for both insurers and consumers. Insurers must prepare for potential market disruptions while consumers face the possibility of significantly higher premiums if enhanced subsidies are not renewed.

No Surprises Act Implementation
The No Surprises Act may have an impact on in-network and out-of-network rates, most notably for care provided by emergency rooms, radiology, anesthesia and pathology. The ongoing implementation of this legislation continues to reshape how insurers negotiate with providers and manage network adequacy requirements.
The law’s impact extends beyond just preventing surprise bills, as it’s forcing insurers to develop more transparent pricing practices and improve provider network management. This is leading to more sophisticated network design and enhanced provider relations strategies.
Looking Ahead: Strategic Implications
For Consumers
Understanding these trends empowers consumers to make more informed decisions about their health coverage. The increased focus on customer experience means better service and more personalized options, while AI integration may lead to faster claims processing and more accurate risk assessment. However, consumers should stay informed about their rights and protections as these technologies evolve.
The expansion of digital health services creates more opportunities for convenient care access, but consumers should ensure they understand how to effectively use these tools and advocate for appropriate care when needed.
For Employers
Employers must adapt their benefits strategies to address rising costs while meeting evolving workforce expectations. This includes exploring innovative plan designs, leveraging technology for better employee engagement, and addressing mental health and climate-related health risks in their wellness programs.
The changing nature of work requires more flexible benefits approaches, with consideration for remote workers, contractor relationships, and varying geographic locations of employees.
For Healthcare Providers
Providers need to prepare for increased use of AI in insurance decision-making, improved data sharing requirements, and changing payment models. The focus on value-based care and population health management requires new capabilities in data analytics and care coordination.
The emphasis on customer experience also extends to provider-insurer relationships, with expectations for more streamlined administrative processes and better communication tools.
Conclusion
The health insurance industry in 2025 is characterized by rapid technological advancement, evolving regulatory requirements, and changing consumer expectations. The integration of AI promises significant operational improvements but requires careful oversight to ensure patient protection. Climate change is creating new categories of health risks that insurers must address through innovative coverage options and risk management strategies.
Rising medical costs continue to challenge affordability, while changing work patterns require more flexible benefits approaches. The emphasis on customer experience is driving digital transformation across the industry, while regulatory changes create both opportunities and uncertainties.
Success in this evolving landscape requires adaptability, innovation, and a commitment to balancing technological advancement with human-centered care. As these trends continue to unfold, stakeholders across the healthcare ecosystem must work collaboratively to ensure that health insurance continues to provide meaningful protection and value for the millions of Americans who depend on it for their health and financial security.

Hi, I’m Hibiki — the writer behind HealthManual.net.
I cover health insurance news, wellness tips, and insightful analysis of pharmaceutical and healthcare stocks. My goal is to simplify complex topics and make health and finance information more accessible to everyone.
Thanks for reading — I hope you find the content helpful and reliable.